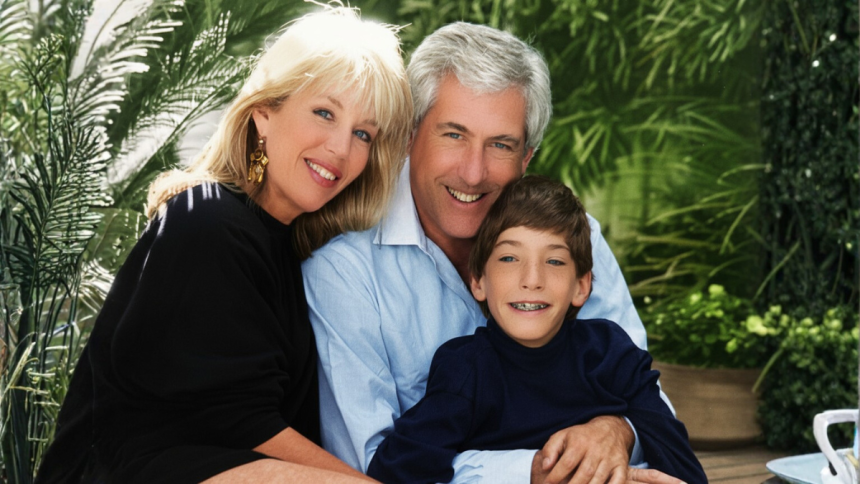
Dementia is often discussed in the abstract — a clinical definition, a list of symptoms, a progression chart. But behind every diagnosis is a family living through a slow and wrenching unraveling. In Losing Richard, author Julie Maxwell provides a deeply human, medically relevant account of dementia’s earliest signs, its misunderstood stages, and the invisible burden placed on caregivers navigating a disease without a roadmap.
Her story is not just emotionally compelling; it is medically important.
The First Silent Indicators Doctors Warn About
Medical professionals often emphasize that dementia rarely begins with dramatic memory loss. Instead, its earliest symptoms are subtle shifts in cognitive processing, executive function, and emotional regulation. Maxwell’s experience illustrates this with striking accuracy.
The first red flag comes on an ordinary morning. Richard — once a disciplined executive and entrepreneur — is found staring blankly at the kitchen counter after losing the puppy’s leash. He cannot articulate what happened. His facial expression is flat, vacant.
This moment is textbook early cognitive decline.
Neurologists refer to these early episodes as “micro-failures of executive function” — brief lapses in planning, organizing, or sequencing tasks. These are often dismissed as stress or distraction, both by families and by patients themselves.
Maxwell writes that she didn’t immediately consider neurological disease. She was grieving her son, managing household duties, and juggling emotional strain. Like many caregivers, she attributed changes in her husband’s behavior to exhaustion.
But over time, the pattern grew.
Behavioral Changes: A Medical Red Flag Often Missed
Doctors stress that dementia is not only a memory disorder — it is a behavioral and neurological syndrome. Maxwell captures this reality in vivid detail.
Richard, once deeply engaged in current events, suddenly stops following politics.
He withdraws from conversations.
He becomes overwhelmed in new environments, especially crowded homes.
He grows frustrated with simple tasks like emptying the dishwasher.
From a clinical perspective, this combination of symptoms signals something far deeper than normal aging.
• Difficulty filtering sensory input
• Diminished tolerance for unfamiliar spaces
• Loss of interest in prior passions
• Emotional dysregulation
These often appear years before a formal diagnosis.
Maxwell’s story supports what medical research repeatedly shows: early-stage dementia is frequently mistaken for depression, burnout, or personality change. Families assume the person is “slowing down,” not neurologically deteriorating.
The Impact of Physical Illness on Cognitive Decline
A key medical element in Maxwell’s narrative is Richard’s 2016 kidney cancer surgery. Although the cancer did not spread, something else changed afterward — subtly, then dramatically.
He healed physically, but the cognitive shifts accelerated.
Fatigue deepened.
Focus dwindled.
Purpose drifted.
Current research acknowledges a strong correlation between major illness/surgery and the unmasking or accelerating of underlying cognitive decline. Post-operative cognitive dysfunction (POCD) is a known phenomenon, particularly in older adults. For some, it resolves; for others, it marks the start of a progressive decline.
Richard’s post-surgical trajectory mirrors the latter.
The Pandemic: A Neurological Pressure Cooker
One of the most compelling medical observations in Maxwell’s memoir involves the COVID-19 pandemic. Isolation, disruption of routine, and sudden loss of structure are known to worsen dementia symptoms.
Richard lost a major consulting job when supply chains collapsed.
His sense of identity shifted.
Social stimulation disappeared.
Neurologists have since documented that pandemic-related isolation contributed to a dramatic cognitive downturn in many older adults. Decreased engagement with familiar environments, reduced cognitive activity, and heightened stress created what some clinicians call “the perfect storm for dementia acceleration.”
Richard’s decline during this period aligns with global observational data.
The Overlooked Patient: The Caregiver
Medical literature has finally begun addressing caregiver health as part of dementia treatment. Maxwell’s story demonstrates why this is not optional — it is essential.
Her emotional exhaustion, hypervigilance, fear, and loneliness mirror what professionals identify as caregiver burden syndrome.
But her hospitalization for five weeks — sudden and life-threatening — highlights a critical reality:
When caregivers collapse, patients collapse with them.
During her absence, neighbors and her sister stepped in. Many families are not so lucky. The medical system still lacks formal support networks for caregiving emergencies — a gap Maxwell’s experience brings into sharp focus.
Why This Memoir Matters for Medical Professionals
Losing Richard is more than a personal story. It is a case study in:
• early detection challenges
• caregiver strain
• post-surgical cognitive changes
• pandemic-related neurological decline
• environmental triggers for confusion
• the need for multidisciplinary support
It illustrates the human impact behind clinical labels, making it essential reading for:
• neurologists
• geriatricians
• social workers
• dementia care teams
• nurses
• mental health professionals
The Final Lesson: Dementia Isn’t Just About Memory
Perhaps the most medically significant message in Maxwell’s memoir is that dementia doesn’t erase a person overnight — it reshapes them.
Richard still enjoys art, familiar meals, quiet cafés, and simple pleasures.
He still smiles.
He still recognizes love, even if he can’t always name its history.
And that reminder — that cognitive decline does not erase humanity — is something both families and clinicians need to remember.